Will Insurance Cover Red Light Therapy?
Will Insurance Cover Red Light Therapy?
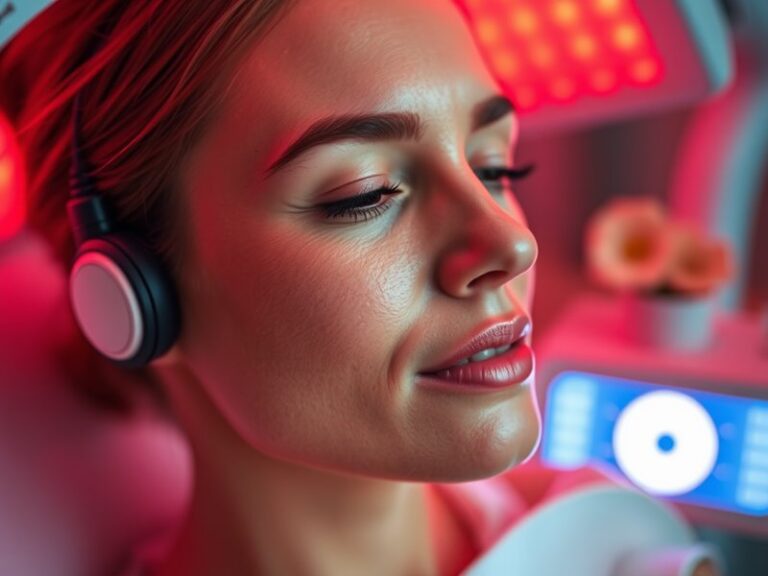
Have you ever wondered if the benefits of red light therapy extend to insurance coverage? This innovative treatment has gained popularity in wellness and pain management, raising critical questions about its reimbursement by insurance companies. In this article, we’ll explore the nuances of insurance coverage for red light therapy, uncover its benefits, and discuss alternatives, helping you make informed decisions about your health.
Key Takeaways
- Red light therapy is often considered a complementary treatment and may not always be covered by insurance.
- Coverage can vary significantly based on insurance providers and specific health conditions.
- Consulting with your healthcare provider can provide clarity on potential coverage and benefits.
What is Red Light Therapy?
Red light therapy (RLT) is a treatment that utilizes low-wavelength light to stimulate cellular repair and regeneration. By penetrating the skin, the therapy aims to enhance healing processes in various tissues, making it appealing for those seeking relief from pain, skin issues, and other medical conditions.
This therapy can involve the use of LED devices or lasers that emit specific wavelengths of light, typically between 600 to 1000 nanometers. RLT is commonly used for several reasons, including:
- Enhancing skin health and reducing wrinkles.
- Alleviating pain and inflammation.
- Supporting muscle recovery and growth.
What are the Benefits of Red Light Therapy?
Red light therapy offers a multitude of benefits across various applications. The following sections will explore these advantages in detail.
Pain Relief
One of the most well-documented benefits of red light therapy is its ability to reduce pain and inflammation. Clinical studies have shown that RLT can effectively alleviate discomfort associated with conditions like arthritis, tendonitis, and fibromyalgia. Users often report less stiffness and improved mobility after consistent sessions.
Skin Improvement
RLT has become a popular treatment in dermatology. It promotes collagen production, helping to reduce the appearance of fine lines, wrinkles, and acne scars. Many users experience improved skin texture and tone, making it a sought-after non-invasive cosmetic treatment.
Faster Healing
Research suggests that red light therapy can accelerate the healing of tissues by enhancing mitochondrial function within cells. This makes it particularly useful for individuals recovering from injuries or surgeries, as it can potentially shorten recovery times.
Read the thorough analysis Does Red Light Therapy Cause Urination?
Enhanced Muscle Recovery
Athletes frequently use red light therapy to expedite muscle recovery after intense workouts. By improving circulation and reducing soreness, RLT has become a vital part of training regimens for many sports professionals.
Is it Possible to Get Insurance Coverage for Red Light Therapy?
While many individuals seek insurance reimbursement for red light therapy, coverage can be challenging. Generally, most insurance companies classify RLT as an experimental or alternative treatment, leading to a lack of coverage in many cases.
What are the Advantages of Insurance Coverage?
If insurance does cover red light therapy, the following advantages may be realized:
- Cost Savings: Insurance coverage can significantly reduce out-of-pocket expenses for patients.
- Access to Treatments: Patients may have greater access to red light therapy as part of their overall treatment plan.
- Guidance with Medical Conditions: Coverage may be more likely for individuals with specific medical diagnoses, ensuring that patients have access to necessary care.
What are the Disadvantages of Insurance Coverage?
The lack of insurance coverage brings several challenges:
- Out-of-Pocket Costs: Patients may have to pay entirely from their pockets, making the therapy cost-prohibitive for some.
- Limited Treatment Options: Patients may be restricted in their choice of providers if coverage is not feasible.
- Inconsistent Policies: Variability in coverage from one insurer to another can lead to confusion and frustration.
What are the Things to Consider Before Seeking Insurance Coverage for Red Light Therapy?
Before pursuing insurance coverage for red light therapy, consider the following factors:
Medical Necessity
Providers often require evidence of medical necessity before approving treatments. Work with your healthcare provider to establish a clear rationale for using RLT in your treatment plan.
Provider Credentials
Ensure that you seek treatment from a licensed and experienced provider. Insurance companies may be more willing to cover therapies performed by certified professionals, adding credibility to your claim.
Read our exploration of Red Light Therapy After Knee Replacement?
Documentation
Keep thorough records of your treatments, including treatment plans, progress notes, and any communications with your health insurance provider. This documentation can be crucial in making a case for coverage.
What are the Alternatives to Red Light Therapy?
If red light therapy isn’t covered by your insurance or is not an option, there are several alternatives worth considering:
Laser Therapy
Similar to red light therapy, laser therapy also promotes healing and pain relief but may have more substantial clinical backing, making it more likely to be covered by insurance.
Topical Treatments
Over-the-counter or prescription topical treatments for skin conditions can be effective and are often covered by insurance, serving as a viable alternative to red light therapy.
Physical Therapy
For those seeking pain relief, physical therapy can provide tailored exercises and treatments, often covered by insurance, addressing issues comprehensively.
Conclusion: Is it Recommended to Seek Insurance Coverage for Red Light Therapy?
While red light therapy offers notable benefits, obtaining insurance coverage can be complex and varies significantly among providers. It’s advisable to consult with your healthcare provider regarding potential coverage, exploring all available options. Balancing the benefits of RLT with its cost implications can help you make an informed decision regarding your treatment choices.
Frequently Asked Questions
Will my insurance automatically cover red light therapy?
Most insurance providers classify red light therapy as a non-standard treatment, meaning that coverage is unlikely without a clear medical necessity backed by documentation.
What conditions may qualify for insurance coverage of red light therapy?
Certain chronic conditions, such as rheumatoid arthritis or chronic pain syndromes, may increase the chances of obtaining coverage if properly documented by your healthcare provider.
Can I file a claim with my insurance for red light therapy?
Yes, you can file a claim by submitting documentation and a letter from your healthcare provider outlining the necessity and intended benefits of the therapy.
Should I consult my insurance provider before starting treatment?
Yes, it’s advisable to contact your insurance provider to understand your specific policy regarding coverage for alternative treatments like red light therapy.
What should I do if my claim is denied?
If your claim is denied, review the reason for the denial, provide additional documentation if necessary, and consider appealing the decision in line with your insurer’s procedures.